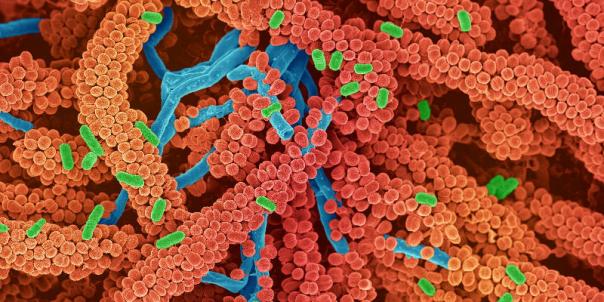
Future prospects for diabetes treatment: Can it be cured? June 20, 2018 Source: Sina Pharmaceutical Diabetes is a chronic metabolic disease characterized by hyperglycemia, often accompanied by metabolic disorders of carbohydrates, fats, and proteins, which are caused by insulin secretion, insulin action, or both. There are two main types of the disease: type 1 diabetes (T1D) and type 2 diabetes (T2D), which account for more than 90% of diabetes. T1D belongs to an autoimmune disease. Due to the patient's autoimmune factors, the beta islet cells responsible for insulin production are destroyed and the insulin is absolutely insufficient. However, in T2D patients, these cells still function, but the body is genetic, obese, and high. Insulin resistance is produced by a calorie diet and lack of exercise. Diabetes is the leading cause of blindness, kidney failure, heart attack, stroke and lower extremity amputation. According to the WHO, diabetes has become a global epidemic with more than 422 million patients, and by 2030 it is expected to be the seventh leading cause of death worldwide. Currently, there is no cure for diabetes. Most medications help to control symptoms to some extent, but patients still face long-term health complications. The biotechnology industry has seen this opportunity and is working hard to develop new diabetes drugs while also striving to develop the ultimate goal of curative therapy. Let's take a look at what is brewing in this area and how it will change the treatment model for diabetes. Type 1 diabetes 1 , cell therapy Although still in a very early stage of development, cell therapy is one of the greatest hopes for developing a cure for diabetes, especially T1D. Replacing the destroyed beta islet cells has the potential to restore normal insulin secretion and cure the disease. However, early attempts to transplant pancreatic cells have largely failed, primarily due to immune responses to donor cells, causing complications and ultimately destroying the implanted cells. In addition, the lack of donors is also a limitation. Currently, one of the fastest alternatives to clinical advancement comes from the Diabetes Research Institute (DRI) in the United States, which is developing a bioengineered micro-organism in which insulin-producing cells are encapsulated in protective barriers. Two years ago, DRI announced that the first patient to be treated in an ongoing Phase I/II trial no longer needed insulin therapy. According to DRI director Camillo Ricordi, this may be the beginning of a new era of islet transplantation, and our ultimate goal is to prevent the need for life-long anti-rejection treatment. In Europe, Viacyte is working with the UK Youth Diabetes Research Foundation (JDRF) to develop a similar device. After Phase I clinically confirmed the safety of the device, the company is currently working to improve the implantation of insulin-producing cells. Several large pharmaceutical companies are also actively involved in the development of their own diabetes cell therapies. For example, Novo Nordisk is developing stem cell therapy and a packaging device, and the company claims that the first clinical trial may be conducted in the next few years. In addition, Sanofi is working with the German company EvoToc to develop a beta cell replacement therapy. A Belgian company, Orgenesis, is also developing a cell therapy in which the cells are implanted from the patient's liver and reprogrammed into insulin-producing cells to avoid problems with the cells from the donor. In the UK, Islexa is developing a similar approach to get cells from the pancreas. Orgenesis's stem cell therapy manufacturing facility Despite the huge potential, these technologies are still far from being listed. First, these techniques must be proven effective in clinical research; secondly, the price can be very high, depending on the application of cell therapy in other areas (such as oncology), the price will reach six figures, and it is difficult to get reimbursement. In particular, considering that diabetes is not an immediate life-threatening disease compared to cancer, health insurance companies in some countries may be reluctant to include diabetes. 2 , against the immune system In T1D, insulin-producing cells are gradually destroyed until completely destroyed, and ultimately the patient is completely dependent on insulin injection. Preventing disease progression in the early stages of the disease, it is possible to preserve these cells and provide treatment for patients diagnosed early. This is the goal of French biotechnology company Imcyse, which is conducting a clinical trial to use an immunotherapy to stop the progression of T1D. In this study, patients who had been diagnosed with T1D and retained some insulin-secreting cells in the past 6 months were treated with an immunotherapy designed to mobilize the body's immune system to destroy the specificity of the insulin-producing cells. Immune Cells. The results of the study are expected to be available later this year, when it will reveal whether this immunotherapy is likely to be T1D. The Belgian company ActoBio Therapeutics is about to start another clinical trial to stop T1D in an unusual way: using a cheese-producing bacterium to deliver two drugs that stimulate regulatory T cells to guide the immune system from attacking Insulin cells. In addition, a T1D vaccine developed by NeoVacs is also about to enter the human clinical, which is designed to delay the progression of T1D after early diagnosis. This approach focuses on reducing the level of an inflammatory protein that is thought to be involved in a variety of autoimmune diseases, including T1D and lupus. 3 , artificial pancreas Attempts to cure or terminate T1D are still in their early stages, and these methods are not suitable for patients whose insulin-producing cells have been completely destroyed. One such solution for this type of patient is to create an "artificial pancreas", a fully automated system that measures blood sugar levels and injects the right amount of insulin into the bloodstream, just like a healthy pancreas. Cambridge University professor Roman Hovorka said in an interview that T1D is a very different disease, the demand for insulin varies greatly every day, and patients can't know what dose they need. Currently, his research team is working on an algorithm that accurately predicts the insulin needs of a particular patient. Replacing humans with computers can give patients better control over blood sugar levels and reduce complications over the long term. A French company, Cellnovo, has confirmed that a partially automated system that monitors blood glucose levels wirelessly but still requires patients to choose insulin levels can reduce the risk of life-threatening hypoglycemia by 39%. The company is currently working with Imperial College, the DigileloopCul consortium and the Horizon2020 program to develop a fully automated artificial pancreas. Type 2 diabetes 1 , induce insulin secretion Kurt Graves, chief executive of Intarcia, a US diabetes company, said in a press release that more than 40 new drugs have been approved for the treatment of diabetes over the past decade. However, the terrible reality is that glycemic control is still poor in most T2D patients. One of the greatest successes in T2D treatment is the glucagon-like peptide-1 (GLP-1) receptor agonist, which induces insulin secretion in islet beta cells and inhibits glucagon secretion. All major giants have GLP-1 drugs on the market or in the research and development stage, including Sanofi, Eli Lilly, Roche, AstraZeneca and Boehringer Ingelheim. On the other hand, Novo Nordisk is also developing an oral version of the GLP-1 drug, which is currently nearing the market. French biotech company Poxel is using a different approach to target the pancreas, liver and muscles with a single drug to help restore the lost function of mitochondria in these areas, and loss of mitochondrial function is thought to drive the progression of T2D. In Sweden, Betagenon and Baltic Bio are developing a first-in-class drug that is expected to simultaneously control blood sugar levels and lower blood pressure, a major risk factor for obese T2D patients. In addition, Morphosys in Germany is also developing drugs to treat obesity in patients with T2D. The company's antibody drug is undergoing Phase II trials aimed at reducing fat, preventing insulin resistance and controlling overeating. 2 , microbiome In the past decade, scientists have realized that the microbes living in our body have a huge impact on our health. Human microbiota, especially the gut microbiota, has been found to be associated with a variety of chronic diseases, including diabetes. At present, scientists have found an unbalanced microbiome composition in diabetic patients, called "disorder", which often reduces the diversity of gut microbiota in diabetic patients compared with healthy people. Researchers from the University of Amsterdam have recently discovered that fecal transplantation, the transfer of a healthy human gut microbiota into the gut of a person with diabetes, can improve insulin resistance in T2D obese patients in a short period of time. Some companies are now beginning to incorporate this concept into their treatment. The French company Valviotis is currently conducting a preclinical test of drugs to increase microbial diversity as a means of treating diabetes. Although promising, the complexity of the microbiome often makes it difficult to establish causal relationships after discovering relevance. It is still difficult to determine the true potential of the microbiome in this field before more diabetes therapies enter clinical trials. 3 , needle-free revolution Intergrity Applications CEO Avner Gal said in an interview that blood glucose testing will be fast and painless in a perfect world. The world may not be so far away, as many companies are developing non-invasive methods to replace fingertip acupuncture. Integrity Applications has developed a device called GlucoTrack that uses electromagnetic waves to measure blood sugar, and the device is available in Europe. Similar technologies are emerging. In London, GlucoSense is using lasers to detect blood sugar levels, while MediWise is using radio waves. Medisise co-founder Panos Kosmas said in an interview that the device can reduce the cost of health care, and in Europe, the annual expenditure on diabetes is 90 billion euros. GlucoWise sensor prototype Patches are also becoming a popular needle-free blood glucose measurement method, such as the FreeStyle Libre, a one-inch wide patch that can be worn for up to 2 weeks. At the University of Bath, researchers are developing a graphene patch that provides greater accuracy by measuring blood glucose levels individually in multiple hair follicles. Other companies are developing implants such as eye implants developed by NovioSense and subcutaneous devices from Senseonic. However, non-invasive blood glucose measurement methods often encounter problems with accuracy. The famous glucose measurement contact lens announced by Google in 2014 is considered “technically infeasible†and needs further development to achieve the accuracy of the fingertip acupuncture method. What is the next step in the treatment of diabetes? Diabetes is a huge therapeutic market and is expected to reach 86 billion euros by 2025 (32 billion euros in the T1D market and 54 billion euros in the T2D market). In the future, we can expect the emergence of revolutionary technologies, including microchips that can diagnose T1D before the onset of disease symptoms, and nanobots that can monitor blood glucose and deliver insulin within the blood vessels. Tomas Landh, director of the strategy and innovation department at Novo Nordisk, said that this is by no means a plot in the novel. I firmly believe that in the next 10 years, micro-robots will become a reality and will become an important part of Novo Nordisk's drug delivery technology. The emergence of such new technologies will undoubtedly have a huge positive impact on the lives of hundreds of millions of people with diabetes worldwide. (Sina Pharmaceutical Compilation/newborn) Article, image reference source: The Future of Diabetes Treatment: Is a Cure Possible? Blood System: Folic Acid Tablet,Iron Drug,Blood System,Enoxaparin Sodium NOUVASANT GROUP LTD. , https://www.nouvasant.com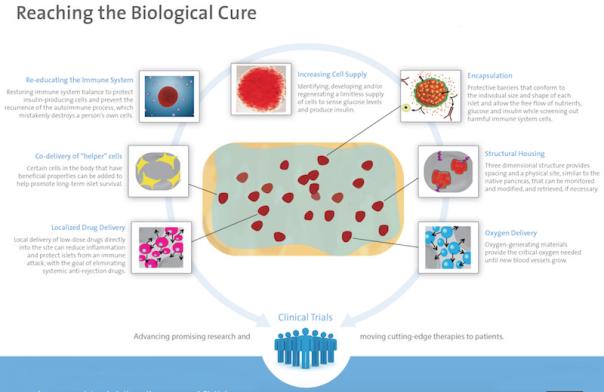




Blood system is also called circulatory system.
For the treatment of diseases of the circulatory system:
According to the American Heart Association, cardiovascular disease is the leading cause of death in the United States. Because of its vastness and critical nature, it is one of the systems of the body most prone to disease.
Pin It Credit: Blood pressure check photo via ShutterstockView full size image
One of the most common diseases of the circulatory system is arteriosclerosis, in which the fatty deposits in the arteries causes the walls to stiffen and thicken the walls. According to the Mayo Clinic, the causes are a buildup of fat, cholesterol and other material in the artery walls. This can restrict blood flow or in severe cases stop it all together, resulting in a heart attack or stroke.
Stroke involves blockage of the blood vessels to the brain and is another major condition of the circulatory system, according to Mitchell Weinberg of the North Shore-LIJ Health System. [Risk factors include smoking, diabetes and high cholesterol," he noted.
Another circulatory disease, hypertension - commonly called high blood pressure - causes the heart to work harder and can lead to such complications as a heart attack, a stroke, or kidney failure, the NLM noted.
An aortic aneurysm occurs when the aorta is damaged and starts to bulge or eventually tear, which can cause severe internal bleeding. This weakness can be present at birth or the result of atherosclerosis, obesity, high blood pressure or a combination of these conditions, according to Weinberg.
Peripheral arterial disease (also known as PAD) typically involves areas of narrowing or blockage within an artery, according to Jay Radhakrishnan, an interventional radiologist in Houston, Texas. In addition, chronic venous insufficiency (also known as CVI) involves areas reflux (or backward flow) within the superficial veins of the lower extremities.
PAD is diagnosed with noninvasive testing including ultrasound, CT scan, and/or MRI. Ultrasound is the least expensive of these methods, but also gives the least amount of detail, as CT and MRI show a much higher degree of anatomic detail when identifying areas of narrowing/blockage within an artery. CVI is diagnosed with ultrasound as the venous reflux can be measured accurately by ultrasound, which ultimately guides treatment.
Future prospects for diabetes treatment: Can it be cured?